Three Things To Read This Week
1. New Research Finds Arrest Rates Drop When Mobile Crisis Teams Respond Instead Of Law Enforcement.
A landmark peer-reviewed study in Psychiatric Research and Clinical Practice tracked outcomes for people experiencing a mental health crisis in five Michigan communities. Over an 11-month period, researchers found that individuals who received help from mobile crisis teams were 45.2% less likely to be arrested than those who received a law enforcement-only response. As the authors note, “only the mobile crisis response [had] a statistically significant reduced incidence rate of arrest,” suggesting these teams “may encourage crisis service pathways outside of 911 and law enforcement, which may decrease … the likelihood of future arrests,” and save law enforcement resources so they can focus on solving serious crime.
The full study is worth your time, but here are the key findings:
Mobile Crisis Teams Significantly Reduced Arrests: “Only the mobile crisis response [had] a statistically significant reduced incidence rate of arrest…[with a] 45.2% lower incidence rate of arrest compared to law enforcement-only recipients…”
Clinician-Led Mobile Crisis Teams—Over Other First Response Models—Made Most Significant Impact: Researchers examined “mobile crisis, co‐response, and office‐ based crisis intervention” crisis teams to mental health calls for service and found that while “all three crisis models showed fewer post-year arrests than their respective law enforcement-only comparisons only the mobile crisis response” had a statistically significant impact on lowering arrest rates.
Mobile Crisis Teams Build Trust, May Help To Reduce Future Arrests: “Mental health service clients and their families prefer non‐law enforcement models, which may increase trust in the mobile crisis team's recommendations…Mobile crisis teams may encourage crisis service pathways outside of 911 and law enforcement, which may decrease risk of future law enforcement contacts or arrests… The findings support the expansion of mobile crisis teams to non‐threatening mental health crises in lieu of law enforcement.”
More On Michigan’s “Reimagining [Of] Mental Health Crisis Response—And [How] It’s Working”:
Dr. Sheryl Kubiak, a dean at Wayne State University, founding director of the school’s Center for Behavioral Health and Justice and co-author of the study above, recently sat down for a sweeping interview with Robyn Vincent, a reporter with Detroit Public Radio and detailed what the state has found over the years after launching these mental health programs that have increased public safety while reducing the burden on law enforcement. Here are some of her key findings (listen to the full interview here):
Mobile crisis response helps reduce cycling in-and-out of jail: “If it is a mobile crisis [team] that’s responding, individuals are much more likely to get into continuing treatment and less likely to end up in jail compared to a law enforcement only approach… They’re not cycling in and out of the jail over and over because they’re in a treatment unit, they’re in the appropriate system.”
Law enforcement responses to mental health calls can escalate crises: “Often what officers are trained to do in the academy is take-control… techniques[,] because they often deal with very unsafe situations. [Those techniques] can actually escalate an individual [in a mental health crisis] and create more psychiatric symptoms that will cause either harm to other individuals… or put the officer in a position where they feel fearful for their own life… [Further] historically, law enforcement officers have not had the training to help them identify when [a call is] a mental health crisis and when it’s ‘bad behavior’ [requiring a law enforcement response].... many law enforcement officers have told us through the years that when they see a person in that level of distress, they believe it’s ‘bad behavior’ [requiring a law enforcement response], particularly before they’ve had the training.”
In Wayne County, “Jail Bookings [Down] By 52%” Since Mental Health Response Started: “The 15,000 mental health calls to 911 [received in a year] — there’s a mental health clinician embedded in 911 now that is fielding those calls, there’s interventions with the behavioral health unit at the probate court, there’s programs at the level of the jail, [and] for law enforcement to recognize behavioral health… Over the past decade, [we’ve been] working to change how we respond to things like mental health crises in Wayne County. It’s having an impact….”
2. New Study: Hospital-Based Violence Intervention Programs “Significantly Reduce Violence-Related Injuries And Recidivism Rates Among Participants.”
A new review of 25 studies examining hospital-based violence intervention programs around the country, published in the scientific journal, Injury, offers the strongest evidence yet that these programs are a powerful public safety tool that, when implemented, “reduce the incidence of violence-related injuries[,] recidivism rates among participants…[as well as] increase employment rates and educational engagement…. [with] cost effectiveness as well as cost savings.” Researchers found that hospital-based violence intervention programs:
Reduce Violence And Arrests: “HVIPs significantly reduced the incidence of violence-related injuries and recidivism rates among participants… demonstrated a significantly lower recidivism rate of 4.4% in HVIP participants compared to non-participants over an 8-year period… Participants who did not participate in HVIP were nearly twice as likely to return with a violent injury…”
Increase Employment, Diplomas: “Improvements in psychosocial outcomes were observed, with increased employment rates and educational engagement reported among HVIP participants… 89% of program graduates either obtained employment, received a diploma, or completed general educational development… participants who gained employment were four times more likely to succeed in the intervention… HVIPs not only reduce recidivism but also bolster long-term socio-economic stability through improved employment and education.”
Save Money: “Implementing HVIPs led to cost effectiveness as well as cost savings from reduced injury recidivism… estimated cost-savings from $82,765 - $4 million across a five-year model…. HVIPs not only enhance clinical outcomes but also extend benefits beyond hospital settings to improve patient employment, mental well-being, and cost savings.”
Momentum For Hospital-Based Violence Intervention Programs Around The Country:
Virginia Hospitals Expanding Hospital-Based Violence Intervention Programming. For the Virginia Mercury, Charlotte Rene Woods reports on state leaders investing $8.5 million on a dozen hospital-based violence intervention programs around the state
“that provide wraparound services and care for violently injured people … in the hospital while they are recovering physically from violence-induced injuries.”
The hospital programs treat victims of violence “like shootings, stabbings and other forms of assault… [and] while receiving medical care for physical injuries, victims are connected to counseling, case management or other community resources… [to help prevent] re-injury or perpetrating violence themselves.” The Virginia programs have treated more than 8,000 people across the state since the programs first launched in 2019, which has reduced violence and saved money—the hospital systems “estimated that over $82 million in health care costs have also been avoided due to preventing and reducing re-injury rates…[with] about $41 million of that is estimated to be direct savings to the state.”Ohio’s New Hospital-Based Violence Intervention Program Shows Early Promise—“Of [The] Patients Enrolled, None Have Fallen Victim To Gun Violence Since. For WLWT, the NBC News affiliate in Cincinnati, Danielle Dindak reports on the City of Cincinnati's new program, launched about a year ago, showing promise with the program enrolling 50 patients and “of those 50 that have enrolled, none have fallen victim to gun violence since.”
Dr. Amy Makley, Trauma Medical Director at UC Health, a champion of the program, explained that the trauma surgeons treat “anywhere from 450 to upwards of 500 victims of gun violence a year,” so there is more work to do, but that the significant early adoption rate of the program shows early signs of promise. When a patient enrolls in the comprehensive program, physicians treat their physical wounds while they are then “paired with a violence prevention professional, screened, and connected to resources…to address issues like housing needs, food insecurity, and mental health support.”New York City Hospital-Based Violence Intervention Programs To “Expand To All Six Of The System’s Level-One Trauma Centers.” The City of New York announced last month that its various hospital-based violence intervention programs—which “ treat over 3,500 patients for violent trauma, about two thirds of whom receive violence interruption, prevention, and community services by HVIP programs”—have now “implemented a unified, multidisciplinary approach to treating victims of violent trauma” across the five participating city hospitals so that they can coordinate and and provide consistent care across the system, and will be “expanding to all six of the public health system’s level-one trauma centers” over the next year.
3. Study: Crime Survivors At Trauma Recovery Centers “Showed Improvement In PTSD, Anxiety, And Depression Symptoms, While Experiencing Lower Rates Of [Re-]Injury.”
In a study published in the peer-reviewed journal AIMS Public Health, researchers at UCLA and the University of Michigan examined 12 peer-reviewed articles evaluating Trauma Recovery Centers in three U.S. locations—San Francisco, Long Beach, and Cleveland—focusing on how these centers serve victims of violent crime.
Researchers found that trauma recovery centers show “promising results for treatment engagement and improvement in psychological and social needs,” with particularly meaningful outcomes for mental health: “Victims of crime who complete at least nine sessions of evidence-based psychotherapy show improvement in psychological symptoms related to PTSD and anxiety” and are “less likely to experience injury recidivism.” Here are the main findings:
Trauma Recovery Centers Dramatically Boost Access to Care: “Access rates range from 55.7% to 72.3%... [and] treatment initiation rates range from 44.0% to 72.0%... [by contrast] other models of care for victims of crime demonstrate rates of treatment initiation as low as 3% … and [only] as high as 14.7% … The rates of treatment access and initiation for victims of crime referred to TRC services are higher than those referred to non-TRC victim services.”
Mental Health Outcomes Improve—Significantly: “Individuals who complete mental health sessions show improvement in PTSD, anxiety, and depression measures… [For example, patients who] meet criteria for PTSD: 72.6% at session one vs. 32.2% at session nine… meet criteria for depression: 68.6% vs. 41.6%... meet criteria for anxiety: 68.3% vs. 46.1%... [and upon treatment completion] “are less likely to experience injury recidivism.”
TRC Services Lead To Better Outcomes Beyond Mental Health: “Assignment to TRC services… mitigated reductions in application for victim compensation in individuals who were ≤ 35 years, had less than a high school education, or were homeless… 55.9% of those randomized to TRC services filed victim compensation claims… [compared to just] 23.0%… receiving usual care… [Of those who filed claims] 78.3% of those receiving TRC services successfully received compensation [versus] 91.5% of those receiving usual care…”
Related: Another paper published last month by researchers at Johns Hopkins University on Trauma Recovery Centers found that the model has proven to “provide comprehensive mental health and case management services to all survivors of violence.” The full paper is worth reading, but here is a spotlight on a vignette from a patient whose recovery was made possible through a trauma recovery center:
“A 20-year-old Spanish-speaking woman is the victim of a home invasion and sustains a stab wound to her leg. She calls 911 and is transported to a hospital. Her stab wound is complicated and will require a specialist. She is discharged from the emergency department to follow up as an outpatient…
…At home, she becomes intensely afraid. She experiences flashbacks of the home invasion. She is unable to sleep, and her anxiety prevents her from leaving the house. She misses her follow-up appointment due to lack of transportation to the specialist an hour away; she is unable to work due to her injury. Her life seems to be spiraling out of control. A friend becomes worried and brings her back to the emergency department to ask what can be done [and is referred to a TRC]...
“...[a] TRC representative arrived at the [ER] bedside to … explain the TRC services, and answer questions. The patient enrolled in both therapy and wraparound case management services. The case manager supported her through conversations with the police and helped her apply for victims’ compensation funds for relocation. The therapist begins working to address her post-traumatic stress disorder symptoms. With the support of the TRC and assistance with transportation options, she can overcome her anxiety enough to engage in her medical care including physical therapy to regain strength. Encouraged by the progress, she completes therapy and, eventually, she can walk steadily and is cleared to return to work…”
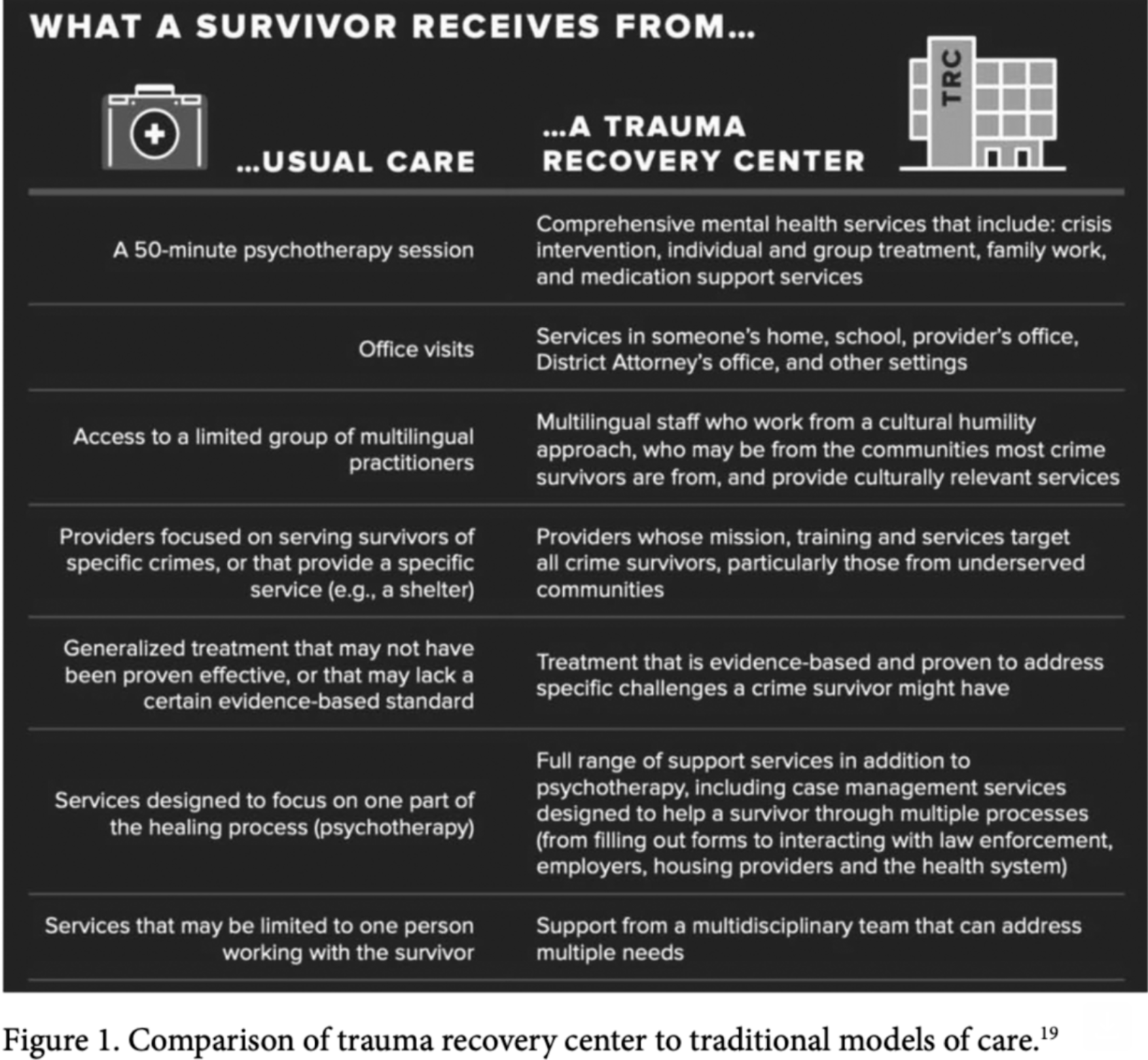
The study also includes a handy infographic about the difference in services from a traditional model versus a Trauma Recovery Center:
More Trauma Recovery Centers Opening Around The Country:
In Arizona, New Trauma Recovery Center Launching For Victims Of Sex Crimes. For KJZZ, Nick Karmia reports on a $60 million recovery center “set to break ground in Glendale… a major step forward in long-term, trauma-informed care.” The facility will “provide 170 beds, including 120 for youths in intensive behavioral health recovery and 50 for survivors facing chronic physical conditions.”
In Kentucky, New Recovery Center Opens In Louisville. For WLKY, Joyce Ogirri reports on the new “state-of-the-art recovery center opening its doors to survivors of “human trafficking and trauma.” The center, “designed for both men and women, offers a comprehensive range of services, including therapy, life coaching, and job readiness training” as well as “addiction recovery, meals, shelter space and much more.”
In Brooklyn, New Center Opens To Help Domestic Violence Survivors. For News12, Rob Flaks reports on a new center opening in Flatbush, a location chosen “due to its [frequent] domestic violence calls and reported violence cases…” The new facility has “therapy rooms, a remote appointment space and child room… [and is] designed to help victims of violent crimes overcome barriers to accessing mental health treatment, health care, and legal resources in the acute aftermath of trauma…”